Edwards Lifesciences’ request for Medicare to cover transcatheter aortic valve replacement in asymptomatic patients with severe aortic stenosis has received support from several medical groups. However, some doctors cautioned against it.
In comments to the Centers for Medicare and Medicaid Services, a debate over expanded use of TAVR centered on results of Edwards’ Early TAVR clinical trial, which showed asymptomatic patients had better outcomes after having the procedure than those in a group that remained under clinical surveillance.
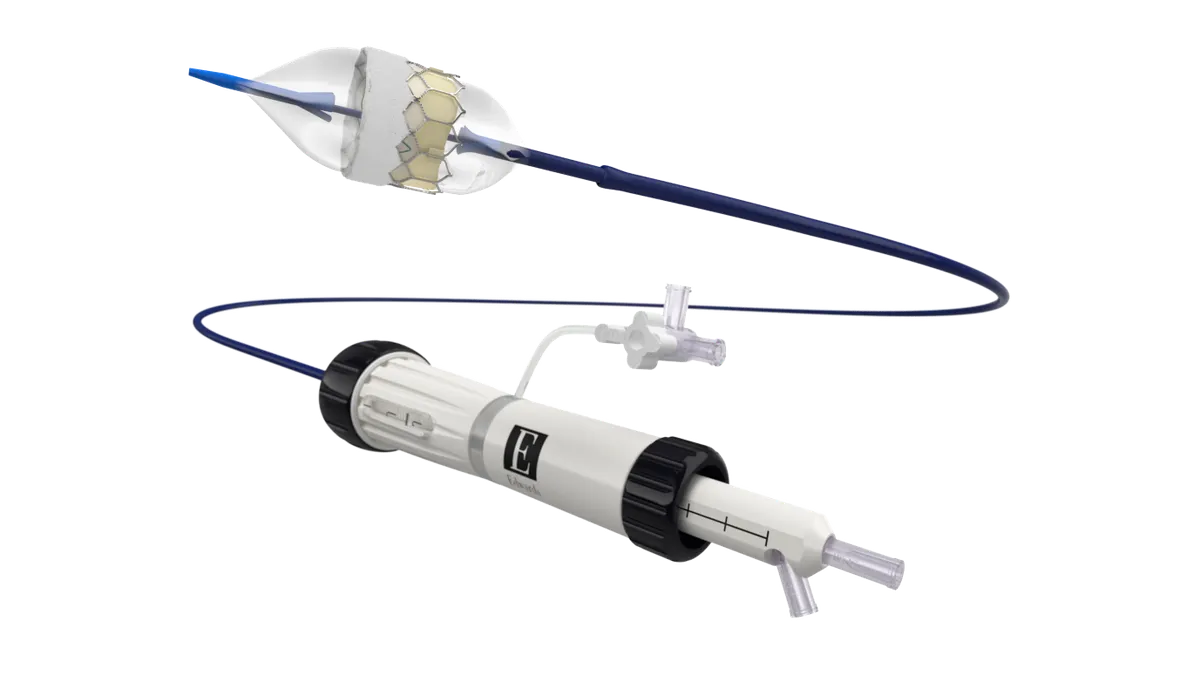
In May, Edwards received the Food and Drug Administration’s approval for an expanded indication for its Sapien 3 heart valve in asymptomatic patients, based on results from the study. The company expects the updated labeling to accelerate sales of the device.
In July, Edwards asked the CMS to extend coverage to Medicare beneficiaries with asymptomatic severe aortic stenosis. The condition is a narrowing of the heart's aortic valve that reduces blood flow to the body.
However, some who recommended against the procedure for patients without symptoms told the CMS more evidence is needed to support expanding its use.
“TAVR may ultimately have a role for asymptomatic patients — but we just don’t know yet,” wrote Steven Woloshin, of the Dartmouth Institute for Health Policy and Clinical Practice. “Until we do, it is premature to change practice.”
Diana Zuckerman, president of the nonprofit National Center for Health Research, said the Early TAVR trial data do not justify broad national coverage because they cannot be generalized to most Medicare beneficiaries. Study participants were predominantly at low risk for surgery.
Earlier implantation of a bioprosthetic valve raises concerns about durability and the risk of repeat interventions over a beneficiary’s lifetime, she said.
“Given the problems with the study design, CMS should be reluctant to make a coverage decision that would encourage Medicare asymptomatic beneficiaries to earlier lifelong device implantation, potential re-interventions, and downstream complications without clear evidence of survival or disability benefit,” wrote Zuckerman.
Debate over updating CED
Edwards also asked the agency to remove requirements for coverage with evidence development, or CED, that it views as creating barriers to care.
CED is a program that allows Medicare coverage while requiring participation in clinical studies.
Joseph Sabik, president of the Society of Thoracic Surgeons, said the group supports an evidence-based approach to treating asymptomatic aortic stenosis and urged the CMS to maintain its CED policy for TAVR.
“While emerging trial data suggests potential benefit in select patients, treatment should be limited to carefully defined populations evaluated by a multidisciplinary Heart Team, with shared decision-making and continued evidence development to avoid inappropriate expansion and overtreatment,” he wrote.
Sabik said CED has been essential for safeguarding patient safety, supporting systematic data collection and guiding responsible expansion of TAVR to new populations. “Removing CED now could compromise the ability to monitor outcomes, address emerging risks, and ensure equitable access to high-quality care,” he said.
Medtronic Vice President Jeff Farkas noted that long-term data are not yet available for the asymptomatic population. “The ability to diagnose asymptomatic aortic stenosis and existing clinical guidelines are not yet mature enough for CMS to use for coverage without additional evidence development,” wrote Farkas.
“While evidence is emerging on TAVR as a treatment option for the asymptomatic aortic stenosis population, we caution that long-term outcomes will be important to establish and monitor for these patients,” he added.
The Society of Thoracic Surgeons, along with four other heart societies, recommended that the CMS update its TAVR national coverage determination to include FDA-approved indications such as treatment for asymptomatic aortic stenosis, and to anticipate future expanded indications such as aortic regurgitation, bicuspid aortic stenosis and moderate aortic stenosis.
“As TAVR has become integral to the care of patients with AS, the impact of an updated NCD will be profound and far-reaching, influencing not only patients who undergo TAVR but also the broader systems of care for all individuals with aortic valve disease,” the groups wrote.
The four additional groups were the American Association for Thoracic Surgery, American College of Cardiology, Heart Failure Society of America, and Society for Cardiovascular Angiography and Interventions.
Edwards Vice President Daniel Lippis maintained that aligning TAVR coverage with approved FDA indications is a priority.
“Edwards believes updating this NCD will not only advance care, but will also improve patient outcomes, provide equitable access for all patients with AS, and reduce long-term Medicare costs,” Lippis wrote.