Dive Brief:
- The Centers for Medicare and Medicaid Services will reconsider its national coverage determination for transcatheter aortic valve replacement in response to a request from Edwards Lifesciences, according to an agency posting on Monday.
- Edwards, in a July letter, asked the agency to reconsider its current policy for TAVR patients who are Medicare beneficiaries to reflect new evidence demonstrating improved outcomes when the valves are used to treat asymptomatic patients. Those patients are currently beyond the scope of Medicare coverage for the treatment.
- Analysts expect expanded Medicare coverage to drive further adoption of TAVR. William Blair analyst Brandon Vazquez said one-third of severe aortic stenosis patients are estimated to be asymptomatic. Broader reimbursement could also prompt more hospitals to open TAVR centers, Vazquez said.
Dive Insight:
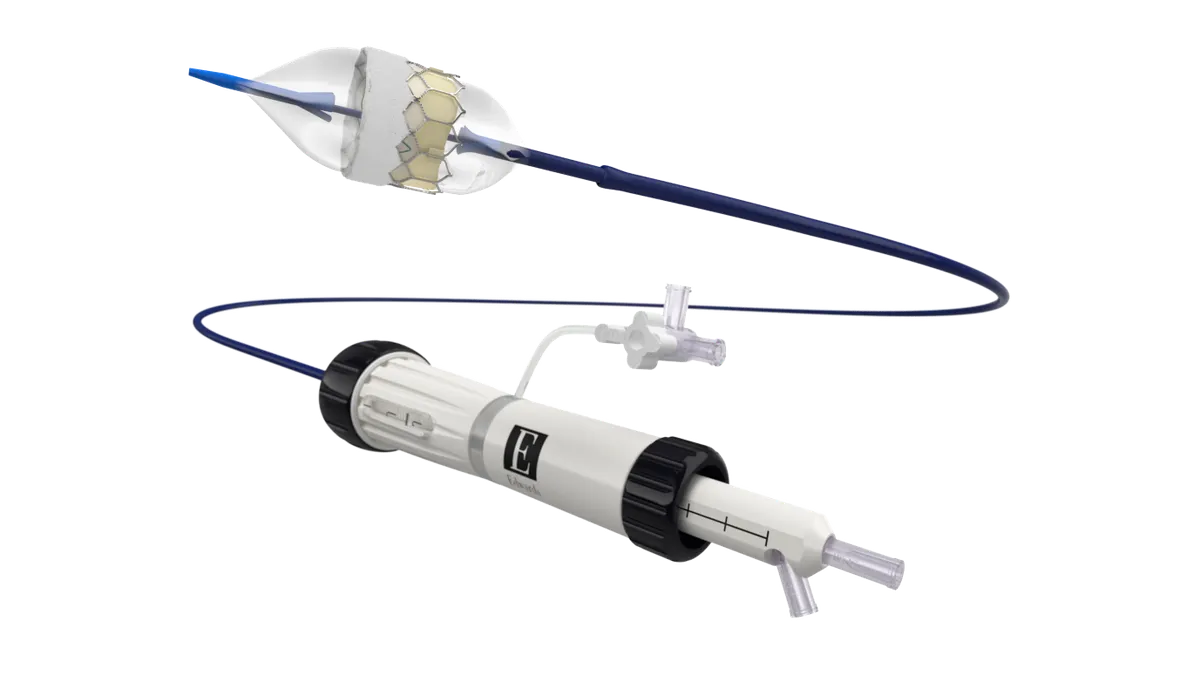
Edwards won an expanded U.S. label indication from the Food and Drug Administration in May for use of its Sapien 3 TAVR devices in people who have severe aortic stenosis without symptoms. The company has also received approval in Europe for the patient group.
The expanded indications reflected results of the valve maker’s Early TAVR study, released in October 2024. The study showed patients with severe aortic stenosis but no symptoms had better outcomes after a TAVR procedure than if managed under clinical surveillance, also known as watchful waiting.
In announcing it will reconsider its TAVR policy, the CMS said it would analyze the clinical evidence for characteristics that make patients more or less likely to benefit from the device and whether specific treatment conditions are necessary to achieve the outcomes demonstrated in studies.
Edwards also asked the agency to remove requirements for coverage with evidence development and other coverage criteria that it views as outdated and creating barriers to care.
BTIG analyst Marie Thibault said Edwards believes that updating the TAVR NCD could help improve efficiency in existing centers. “We agree and think there may also be some opportunity to add new TAVR centers,” the analyst wrote.
The CMS said it expects to issue its proposed decision memo on Edwards’ request by June 15, 2026, and complete the national coverage analysis by Sept. 13, 2026. Public comments will be accepted until Jan. 14, 2026.