Dive Brief:
- A coalition of more than 30 trade groups from across the healthcare industry is calling on Congress to pass legislation that would prevent steep Medicare reimbursement cuts for laboratory testing services from taking effect in January.
- In a letter sent last week to congressional leaders, groups including AdvaMed, the American Clinical Laboratory Association, the American Medical Association and the American Hospital Association said the legislation is needed to stabilize Medicare payments for diagnostics set under the Medicare Clinical Laboratory Fee Schedule, or CLFS.
- The organizations support a bill called the Reforming and Enhancing Sustainable Updates to Laboratory Testing Services Act, or RESULTS, that would direct the Centers for Medicare and Medicaid Services to contract with an independent, not-for-profit commercial claims database to set CLFS rates for widely available tests.
Dive Insight:
The RESULTS Act was introduced in September in both the House and Senate with bipartisan support. It aims to reform the CLFS rate-setting process established under the 2014 Protecting Access to Medicare Act, or PAMA, and thereby stop payment reductions of up to 15% that are scheduled to take effect Jan. 1 for about 800 lab tests.
Such cuts threaten patient access to routine and life-saving diagnostic tests, the groups said.
PAMA was intended to create a national fee schedule, based on private market data, reflecting a range of labs that serve Medicare beneficiaries. However, industry groups contend that PAMA created a process that sets reimbursement rates artificially low, resulting in nearly $4 billion in cuts from the CLFS in the first three years.
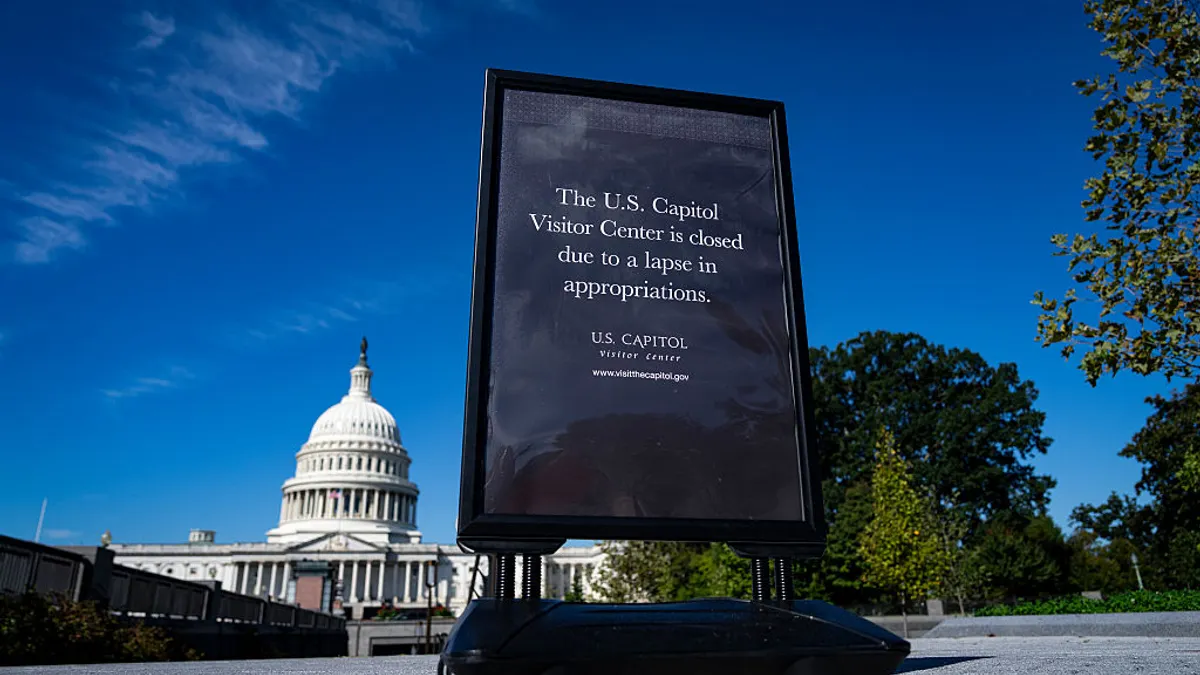
Congress has acted to delay payment cuts in each of the last five years. The healthcare groups argue it is time to enact permanent reform through the RESULTS legislation. Their plea comes amid a federal government shutdown that is on track to become the longest in U.S. history.
ACLA said CLFS rates for widely available tests would be based on robust private payer claims data, while clinical labs would be required to report commercial rate data directly to the CMS for tests that are not widely available, such as proprietary diagnostics and those for rare diseases.
In addition to revamping the rate-setting process to reflect up-to-date market information, the bill is intended to reduce the data collection and reporting burden on clinical labs and the administrative burden on the CMS by extending the rate-setting cycle to every four years.
It would also establish limits on annual payment reductions and exclude artificially low Medicaid managed care payment rates from the data used to set reimbursement levels.