At the Transcatheter Cardiovascular Therapeutics conference in San Francisco this week, Edwards Lifesciences’ patient outcome results seven years after receiving transcatheter aortic valve replacement were among the most closely watched data.
Interventional cardiologists gathered at the meeting also heard from Philips, which examined the treatment of additional blockages in heart attack patients, and Penumbra, whose study compared mechanical thrombectomy plus blood thinners to anticoagulation therapy alone for patients with pulmonary embolism.
Here are three key updates from the conference, which is the annual scientific symposium of the Cardiovascular Research Foundation:
1. Edwards TAVR vs. SAVR at 7 years
Seven-year follow-up data from Edwards Lifesciences’ PARTNER 3 TAVR trial evaluating low-risk patients with severe aortic stenosis showed TAVR was not inferior to surgery.
The primary endpoint of composite death, stroke or rehospitalization at seven years demonstrated non-inferiority between TAVR and surgical aortic valve replacement, at 34.6% for TAVR and 37.2% for SAVR.
The analysis, published Monday in The New England Journal of Medicine, also showed the percentage of bioprosthetic valves that failed was 6.9% in the TAVR group and 7.3% in the surgery group.
Mortality from any cause was 19.5% in the TAVR arm and 16.8% in the SAVR arm, and the percentage of patients with stroke was 8.5% in the TAVR arm and 8.1% in the surgical arm.
J.P. Morgan analyst Robbie Marcus said that heading into the presentation, investors were concerned about a potential widening mortality curve for TAVR. Trends in mortality and stroke bear watching, said the analyst.
“However, with a non-inferior result on the primary endpoint alongside good valve durability, we don’t expect any meaningful changes to clinical practice,” Marcus wrote Monday.
2. Philips looks at artery treatment after heart attack
A study of heart attack patients showed that additional blockages in arteries can safely be treated in the same procedure addressing the acute event, rather than being deferred, according to Philips.
When patients suffer a serious heart attack, cardiologists typically open the blocked artery causing the attack, but additional narrowed arteries are not treated right away, due to time constraints, patient stability or because they go unnoticed.
In the iMODERN study, patients were randomly assigned to immediate physiology-guided treatment of additional narrowed arteries during the first procedure using instantaneous wave-free ratio, called iFR, or staged treatment guided by cardiac magnetic resonance imaging four days to six weeks after the heart attack.
After three years of follow-up, the trial found no significant differences in death, repeat heart attack, or hospitalization for heart failure between the two approaches. Serious adverse events occurred in 145 patients in the iFR group and in 181 in the MRI group.
“These results address one of the longest-standing questions in interventional cardiology,” Niels van Royen, co-principal investigator of the iMODERN trial at Radboud University Medical Center, Netherlands, said in a Philips statement.
The iMODERN study enrolled 1,146 patients at 41 hospitals in 14 countries. Results were published Tuesday in The New England Journal of Medicine.
3. Penumbra study yields favorable outcome
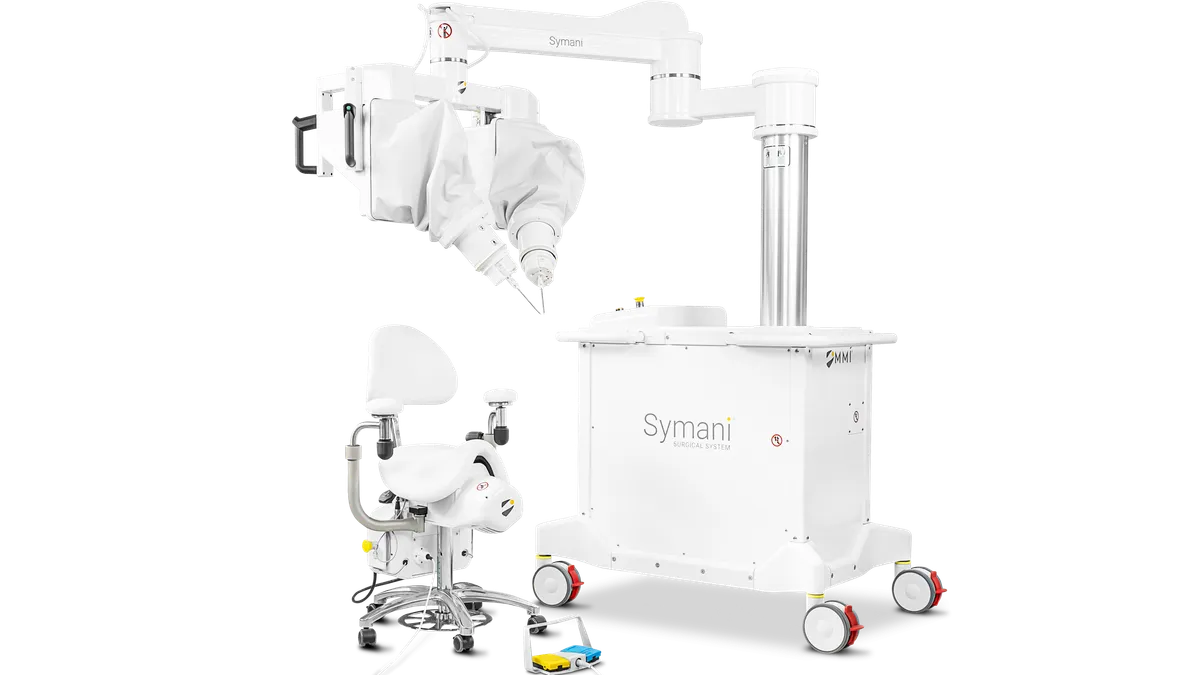
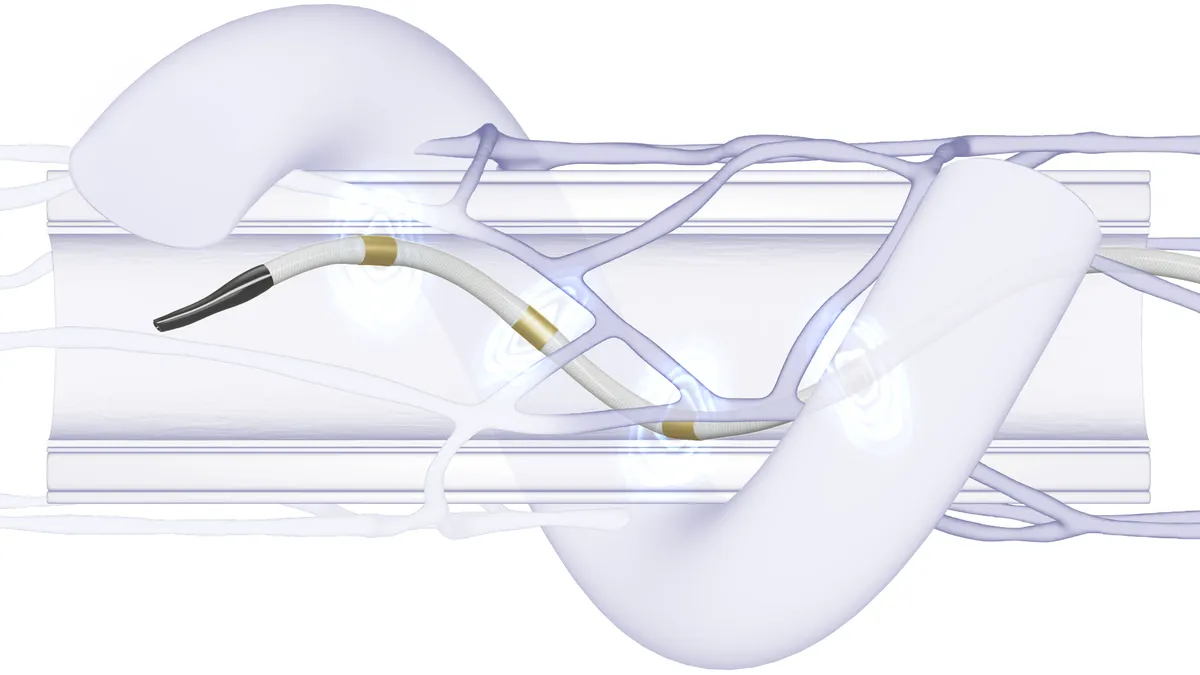
Penumbra’s mechanical thrombectomy treatment combined with anticoagulation therapy was superior to blood thinners alone in reducing right heart strain in patients with intermediate- to high-risk pulmonary embolism, according to a study of 100 patients at 22 sites.
The findings of the STORM-PE trial suggest the device can quickly help to improve recovery of the right heart, Robert Lookstein, a principal investigator of the study and professor of radiology and surgery at Icahn School of Medicine at Mount Sinai, said in a Penumbra statement.
In the randomized, controlled trial, patients treated with computer-assisted vacuum thrombectomy plus anticoagulation saw a 29.7% relative reduction in right heart strain within 48 hours, compared with a 13.1% reduction for those who received anticoagulation alone.
Improvement was achieved without an increase in complications. The rate of major adverse events within seven days, measured by a composite including PE-related mortality, recurrent PE, clinical deterioration requiring rescue therapy and major bleeding, was comparable between the two patient groups, at 4.3% with the device treatment versus 7.5% for anticoagulation alone.
William Blair analyst Brandon Vazquez, in a note Monday, said the data hit the key metrics he was looking for and should help speed adoption of Penumbra’s Lightning mechanical thrombectomy technology.