Dive Brief:
-
Healthcare payer trade group America’s Health Insurance Plans (AHIP) has accused out-of-network test providers of price gouging in COVID-19 testing, the latest in the debate over the cost of tests and who is paying for them after Congress mandated that patients pay nothing out of pocket.
-
At the same time, clinical laboratory trade group ACLA last week said tri-agency guidance has "significantly eroded" protections Congress put in place to ensure COVID-19 tests are fully covered by insurers. ACLA cited a letter sent in late October by bipartisan lawmakers to HHS Secretary Alex Azar that said health plans are increasingly denying coverage for COVID-19 tests, with denials for asymptomatic individuals common.
-
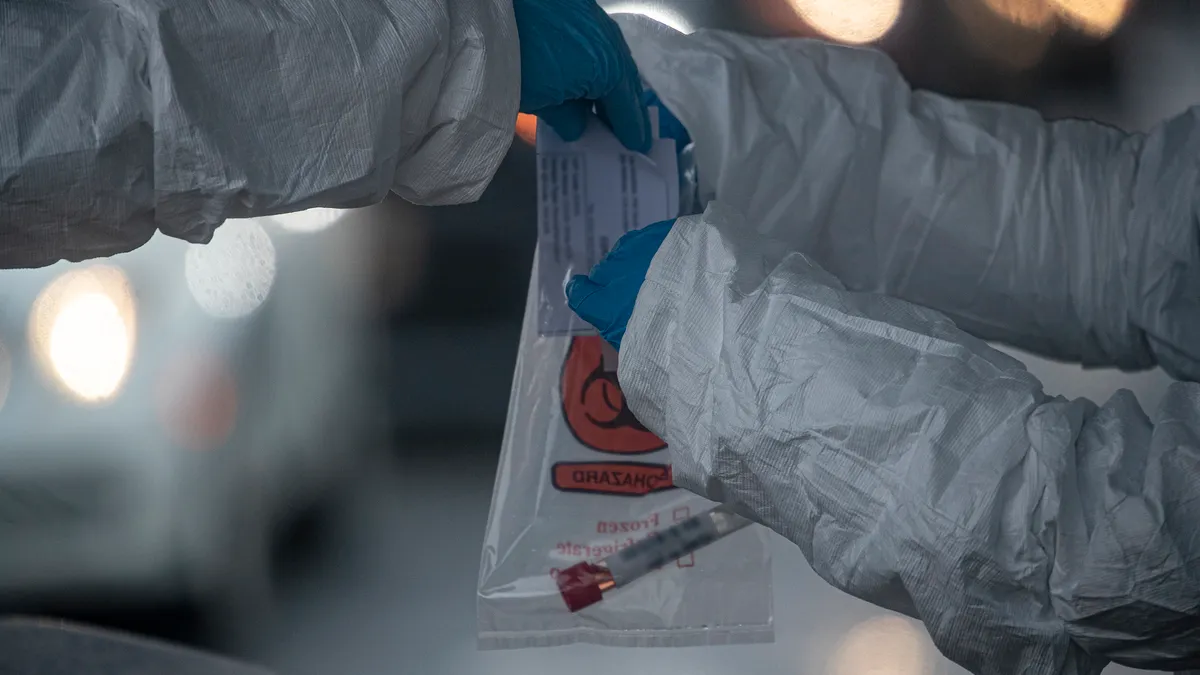
ACLA's call for the expansion of COVID-19 testing coverage came days before the New York Times provided updated reporting on surprise bills received by some patients charged "facility fees" of more than $1,000 for being tested in tents outside of hospitals or in drive-through services. An ACLA spokesperson said these are the kinds of healthcare provider "bad actors" that are taking advantage of the situation.
Dive Insight:
The Families First Coronavirus Response Act and the Coronavirus Aid, Relief, and Economic Security (CARES) Act both included provisions ensuring that individuals can receive COVID-19 tests without out-of-pocket costs. However, ACLA says "murky" regulatory guidance issued in June by HHS, Labor and Treasury is driving coverage denials and high costs.
The trade group for LabCorp and Quest Diagnostics argues that guidance "muddied the clear coverage mandates passed by Congress that require group health plans and health issuers to cover COVID-19 testing without cost sharing or prior authorization."
"Without federal assurance that COVID-19 tests will be covered by insurance plans, patients continue to face a patchwork system that drives uncertainty and undermines federal response efforts," Julie Khani, ACLA's president said in a statement.
AHIP, which represents big payers like Aetna, Anthem and Humana, made the price gouging accusation against out-of-network test providers after their survey of health insurers found almost half of out-of-network claims for PCR tests cost $185 or more, well above the average of $130 charged by in-network providers.
With the situation worsening in recent months, AHIP called for Congress to set "a reasonable market-based pricing benchmark" for out-of-network tests.
In July, an AHIP survey found 39% of out-of-network claims for PCR testing exceeded $185. AHIP set $185 as the threshold for price gouging as it is 50% above the $130 typically charged in network. At that time, 9% of all claims were coming from out-of-network providers.
The October survey identified changes in the role played and claims made by out-of-network test providers. In that poll, 47% of out-of-network claims exceeded $185. The increase was mainly due to an increase in the proportion of providers claiming $185 to $260. That figure increased from 18% to 23% between the two surveys. The proportion of out-of-network providers claiming more than $260 rose from 21% to 24%. More than 10% of providers continue to claim in excess of $390.
AHIP tracked increases in the price of antibody tests, too. At the last count, 34% of out-of-network claims for COVID-19 antibody tests exceeded the in-network average by 50% or more. In July, the figure was 25%. The October survey saw a jump in the number of out-of-network claims in excess of $390. AHIP also identified perceived overcharging for antigen tests.
The impact of price rises on insurers was magnified by increased use of out-of-network testing. The latest survey found 23% of all COVID-19 claims came from out-of-network providers, up from 9% in July. Most of the $185-plus claims submitted by out-of-network providers came from standalone laboratories.
AHIP is asking Congress to set a market-based pricing benchmark for out-of-network tests and provide money to ensure Americans can access COVID-19 tests.
ACLA is also in favor of federal funding for broader access to testing. The clinical lab trade group, along with AHIP and nearly 50 other stakeholders, in July sent a letter to Senate and House leaders calling for a dedicated federal testing fund.
Without such funding, and the number of U.S. coronavirus cases surging, ACLA, AHIP and other groups say there will be disruptions in clinician, hospital, and lab payments as well as higher insurance premiums.