The promise of AI in healthcare is finally starting to move beyond speculation.
In recent years companies have been funneling funds into advancements, especially those that seek to cut costs and promote patient health. Spending on healthcare AI technology is expected to surpass $34 billion by 2025, compared to $2.1 billion in 2018, according to market intelligence firm Tractica.
Amazon, Siemens, IBM, Optum and GE Healthcare and health systems Mayo Clinic, Memorial Sloan Kettering and Intermountain are mining patient records for health data to train AI algorithms, allowing the machines to learn by recognizing patterns and make key predictions.
In some cases, such deep learning systems are already outperforming doctors. In others, they're not.
Either way, experts predict that in 2019 AI in healthcare will continue to grow — especially in the areas of imaging, diagnostic, predictive analytics and administration.
Administration — scheduling, operations, billing — is the biggest area for AI growth in the coming months
The AI for healthcare information technology market is expected to exceed $1.7 billion by the end of 2019 alone. That tech can be used to detect the waste, fraud and abuse in healthcare spending — estimated between 3-10% of the more than $3 trillion spend in the county every year.
Frost and Sullivan's SVP of Healthcare and Life Sciences Reenita Das predicts operationalizing AI platforms across healthcare workflows would result in a 10-15% productivity gain over the next couple of years.
In the current healthcare environment, with skyrocketing costs, an aging population and workplace shortages, it's important to leverage use cases that aren't clinical, Intel's worldwide head of the health and life sciences group Jennifer Esposito told Healthcare Dive.
Repetitive, time-consuming tasks are where AI thrives — and there are a lot of those in America's healthcare chassis. "We're seeing a lot more of a conversation shift to AI being an augmenter or an enabler or an assistant," Esposito said.
One example is scheduling and appointments. Cleveland's MetroHealth System had a 10-35% no-show rate at its four hospitals before bringing AI into its operational decision-making in late 2017.
MetroHealth used AI to quantify that select patients that had a high likelihood of not showing and double book those patients in order to not waste providers' time, MetroHealth's chief strategy and innovations officer Karim Botros said at a 2018 U.S. News Healthcare of Tomorrow panel on AI.
The AI practice operates in the background, integrated into MetroHealth's Epic system. So far, it has reduced the next available appointment time by roughly 30%, according to Botros.
Hospital operations is another place AI may help in 2019, experts say, by predicting where in the hospital workers are most needed.
Cleveland Clinic is currently tracking hospital bed use through an AI platform initially built for retailers. It keeps tabs on its surgical suite resources to get to full capacity and utilization. The program looks at patient movements through the OR to help identify potential bottlenecks in that process.
AI can also be leveraged to keep track of drugs and medical devices in health facilities, along with promoting financial responsibility in patients.
Kit Check sells machine learning to help hospitals identify drug diverters. Called Bluesight for Controlled Substances, it identifies high-risk hospital employees who may be stealing drugs by scoring them on a range of metrics, such as physical location, documentation and timing behaviors.
Scoring is based on "your peer group and on your hospital to basically figure out if you're unusually high or unusually low" in terms of risk, CEO and co-founder Kevin MacDonald told Healthcare Dive.
And artificial intelligence may be helpful for reducing drug spend altogether, MacDonald said, especially in the areas of controlled substance waste, drug spend and safety and compliance.
AI could become more prominent in billing platforms in the coming months as well, predicts software-as-a-service company Simplee's CMO John Dwight.
Simplee sells data and predictive analytics to determine a patient's ability to pay a bill in a hospital's payment portal. It then automatically recommends a payment plan or payment options that fit the patient's financial profile.
"The first thing we see is online payment plan generation goes up a lot. The second thing we see is patient satisfaction goes up," Dwight told Healthcare Dive, stressing that in the longer term collections for the health system increased as well.
But when bringing in any new tech shift, providers need a clear understanding of existing workflows and how to optimally adjust them, Esposito said.
"Where we've seen a lot of health systems and others run into issues is when you're really just trying to tack something on without really thinking about the workflow, the culture and an understanding of when it's really working or not," she said.
Streamlining patient matching, population health management and accessibility
Artificial intelligence chatbots and virtual assistants, like Babylon Health's disease prevention and diagnostic AI, Sense.ly's virtual nurse platform Molly and Novo Nordisk's diabetes chatbot Sophia, promote accessibility and can steer nervous patients away from an unnecessary visit.
If patients need care, AI can help them be paired with the appropriate clinician.
Hospital giant Providence St. Joseph Health uses AI tech called Kyruus to improve the chances of matching patients with the right provider. Before it started using the tech, about 30-40% of appointment slots had been empty or poorly used, PSJH chief data officer Aaron Martin said at the U.S. News Healthcare of Tomorrow conference in November.
Kyruus uses a provider data management program to identify, match and book patients appointment with specialists most fitted to meet their needs.
More seniors are preferring to age in place, and AI modifications can create smart homes to keep an eye on seniors' health and safety, predicts Philip Regenie, CEO of artificial intelligence healthcare company Zanthion.
But AI at-home monitoring isn't just for seniors.
Experts predict that this year AI will continue to drive the shift in healthcare from being a reactive and hospital-based model to a proactive and home-based one. Advancements in AI will be especially helpful for patients with chronic conditions or limited mobility.
In tandem with home sensors, wearables and other at-home treatment plans, AI may help detect serious illnesses prior to becoming symptomatic.
AccuHealth, a care management company based in Chile, collects patient data using a variety of sensors in the home and feeds it into its AI engine to build predictive alerts and models.
If an alert is triggered, a remote virtual hospital force can intervene with those patients and their families to avoid a potentially irreversible decline in health (and an expensive emergency room visit).
Anthem is six months into a year-long partnership with doc.ai, testing whether blockchain-enabled AI can predict when people will experience allergic reactions based on data such as age, weight, height, physical activity and pollution exposure.
AxisPoint Health, an analytics-based care management and population health management services provider, uses traditional (claims, eligibility, provider) and nontraditional (consumer) data to identify proxies for social determinants of health. It feeds that data into a decision support and workflow platform to present care managers with comprehensive profiles and health predictions for its patients and populations, using predictive analytics to identify risk for up to a year.
For example, "if there's a wildfire in the area and there are high particulates in the air, then there can be blast messaging going out to individuals with respiratory conditions to keep the windows closed and avoid exposure to the smoky air," Virginia Gurley, SVP and CMO of AxisPoint, told Healthcare Dive.
Optum, UnitedHealth's pharmacy benefit management and data analytics arm, is developing a prototype mobile app called MyDigitalTwin to minify sensor architecture from the home or facility to the body itself. The model leverages massive amounts of genomic, exogenous and behavioral data to create an online representation of a person's health.
"Imagine if each of us had a digital twin our doctor could use to model our current health, predict our future health and pinpoint suggestions to improve our health," Kerrie Holley, a technical fellow at Optum, said at the company's August forum about the real-time modeling software.
But this area is still in its infancy. "I believe that the full potential [of predictive modeling] is still on the horizon because physicians and insurers (in particular) still need to be convinced of the benefit," Global Data's global head and EVP of Healthcare Operations and Strategy Bonnie Bain told Healthcare Dive.
Insurers can see potential cost savings, too
Accenture predicts AI could save U.S. insurers about $7 billion in just 18 months by streamlining core functions such as billing, enrollment, claims, quality and compliance and customer service.
One example of the latter is Afiniti, a tech company that leverages predictive analytics to pair customers with call center operatives based on subtle patterns in human behavior from client and commercially owned data.
"One of the major drivers of mortality and morbidity in a population is whether or not they get regular visits from a nurse practitioner," Zia Chishti, Afiniti's CEO, told Healthcare Dive. Insurers, including giant UnitedHealth, use Afiniti's tech to improve the likelihood of that outcome.
Afiniti's healthcare clients have seen $125 million in savings on the payer side since 2017.
For payers, the potential of AI is about "taking some of the simple things people ask about and answering them without human intervention, being able to anticipate need," Richard Birhanzel, managing director of Accenture's payer business, told Healthcare Dive in August.
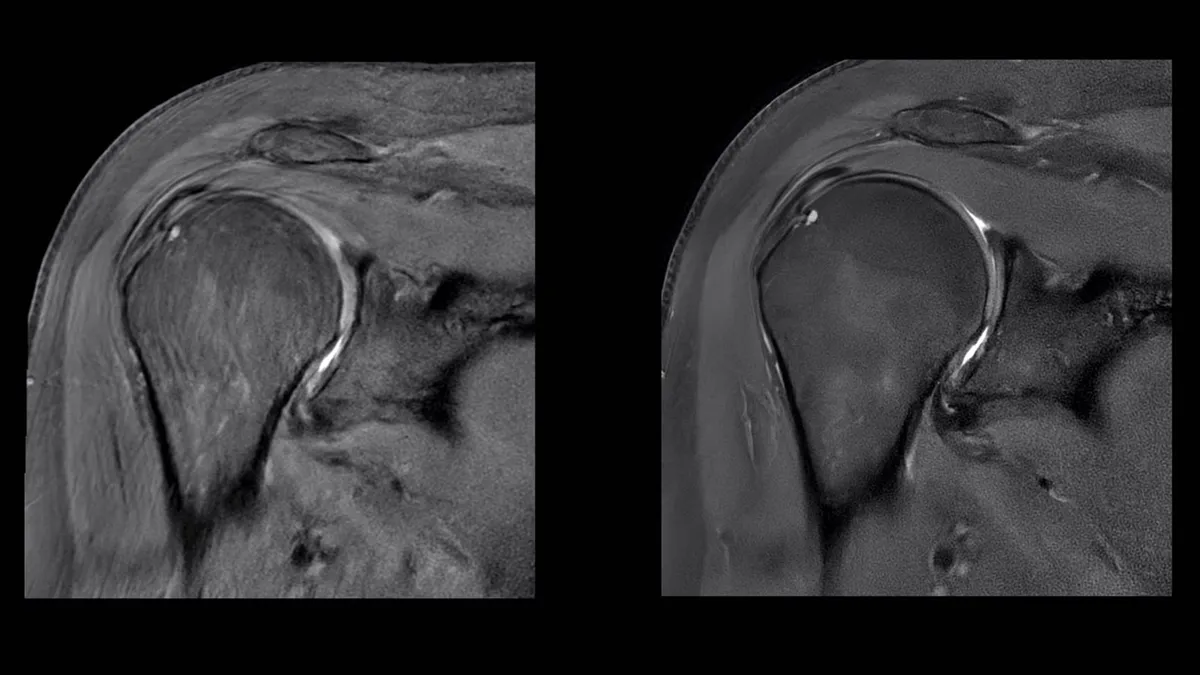
Steady growth in imaging, diagnostic capabilities
The healthcare sector became much more used to AI's applications in radiology and image analysis in 2018, and that's almost certainly going to continue into the new year.
The impact of AI is evident in such image-intensive arenas of medicine like pathology, dermatology and radiology. Of the more than 100 AI for medical imaging startups last year, the clear majority focused on image analysis, according to healthcare consultancy Frost & Sullivan, and the AI-based medical imaging market is on track to reach $2 billion by 2023.
But the healthcare community has looked at AI in diagnosis with a healthy dose of skepticism, especially following the IBM-Watson debacle earlier last year when the supercomputer failed to properly detect or provide treatment suggestions for cancer.
The tech reached too far too quickly, experts say. But there's serious potential for AI in very specific diagnostic areas moving forward.
For example, AI in tandem with EKG can be successful at detecting a form of heart disease, according to the Mayo Clinic. And Scripps teamed up with NVIDIA to develop deep learning tools to predict atrial fibrillation (and analyze whole genome sequences) in October.
Memorial Sloan Kettering and Stanford University are both looking at the applications of machine learning in oncology.
Recently, a team of researchers from Beth Israel Deconess Medicare Centre and Harvard Medical School used deep learning to train an AI to diagnose tumors. When combined when human pathologists, the program reached 99.5% accuracy.
AI diagnosing on its own is within view — for eye diseases, at least — but it's unlikely to ever replace humans altogether
In August, Google announced that its DeepMind AI system recommended the proper eye referral for more than 50 eye diseases with 94% accuracy — on par with specialists, though the tech is not yet clinically approved.
That trophy has already been snagged by IDx-DR. In April, the software became the first autonomous AI to be commercially authorized by the FDA for diagnosis of diabetic retinopathy, a complication of Type 1 and Type 2 diabetes that can lead to eventual blindness.
IDx founder and CEO Michael Abramoff spent eight years working with the FDA to get his software approved. "For them it was new because no one has ever come to them with an idea for an autonomous AI, meaning an artificial intelligence that makes a clinical diagnosis, or a therapeutic diagnosis, by itself," Abramoff told Healthcare Dive.
Autonomous AI has wide-reaching implications, especially when it comes to patient access. The tech allows users to run extremely niche diagnostics and therapeutics in neighborhood retail clinics, for example, where it's difficult to find highly qualified specialists.
The drawback, though, is that AI can only be applied to diagnose very specific types of diseases. The condition needs to be common and present similar symptoms each time, Abramoff said.
Some diseases that meet the benchmarks are glaucoma and macular degeneration. Outside of the eye, companies are exploring the applicability of autonomous AI in gastrointestinal tract and skin conditions as well.
One exploratory example of the latter is Doctor Hazel, an app that sorts through a database of images to classify moles as benign or potentially cancerous, introduced at TechCrunch Disrupt in 2017 and since renamed BlueScan.
Abramoff expects many more announcements in 2019 around AI as a diagnostic tool, but stressed that autonomous AI does not mean AI outside of human hands.
"Doctors make errors," and "the AI will make errors," Abramoff said. "The AI we're working on is still embedded in the healthcare system" — human and tech working in tandem.