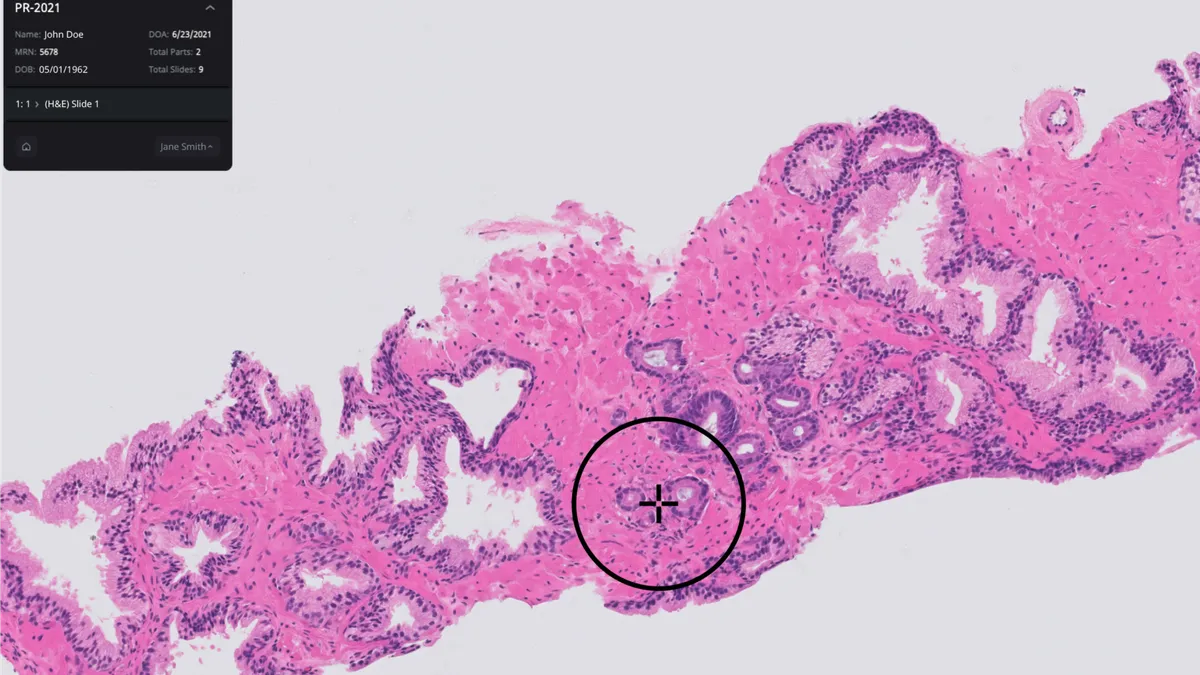
As artificial intelligence makes its way into hospitals and laboratories, pathologists are starting to use software tools to help with cancer detection.
New York-based Paige has developed a number of computer-aided tools to screen for cancer. In September 2021, the company received de novo clearance from the Food and Drug Administration for a software tool that can flag potential prostate cancer cases in tissue slides, the first product of its kind.
Paige, launched in New York’s Memorial Sloan Kettering Cancer Center, was founded by Thomas Fuchs, who leads MSK’s computational pathology group, and David Klimstra, who previously served as chair of the hospital’s pathology department. Their first product, Paige Prostate Detect, was trained on 60,000 slide images and validated on another 40,000 to identify potentially cancerous areas.
The company has since built a suite of products for breast cancer, which haven’t yet been cleared by the FDA, and it has partnered with commercial laboratories and academic medical centers including Sonora Quest, The University of Louisville, Quest Diagnostics and Inform Diagnostics.

In January, Andy Moye became CEO of Paige after working as the company’s chief commercial officer and leading commercial operations for Philips’ digital pathology solutions in the Americas. In an interview with MedTech Dive, he shared his plans for the company and talked about what it will take for more laboratories to use digital pathology tools.
This interview has been edited for length and clarity.
MEDTECH DIVE: You became CEO of Paige in January. Where are you looking to take the company?
ANDY MOYE: We see the company still moving in the same direction. We're excited to still be the only [pathology] company out there with an FDA approval for AI technology, with Paige Prostate [Detect]. It's been a whole year at this point and no one else has been able to replicate that achievement. We're extremely proud of that.
We're continuing to work on regulatory filings for AI tools that really enable pathologists to do their jobs better, faster and more efficiently, with better quality, with patient care in mind, so that you're getting better patient outcomes.
We're also very excited about the transformative side of AI in tissue, with bringing out biomarkers. Something like HER2Complete, which we recently announced a CE Mark on, which allows the pathologist to say is there actually some mRNA expression in this tissue, and being able to see if the AI can predict that right from the [biopsy] slide.
How are you approaching the regulatory process with the FDA?
The FDA really regulates the full chain, [from] the pixel when that slide is scanned, all the way through to when it's reviewed by a pathologist on the screen so that nothing is lost. I was with Philips when Philips got the first ever FDA [clearance] for the [ultra-fast pathology slide] scanner, and that was a full end-to-end solution, the scanner plus all the IT and the infrastructure and the monitor, everything.
That particular approval for us is modular. To be a full FDA workflow, we have to have an FDA-approved scanner. But then we can pick up that image from that scanner, and should another scanner get FDA approval, we’ll work with the FDA to get our viewer cleared through that process. When you have an AI application, it's the same thing. You have to have the same pixel flow, scanner to viewer, then AI application on top of that.
We really did break new ground there with the FDA. They simply had never regulated anything like this before and so they had to create a group within the FDA to do this. We were able to set the bar pretty high when it came to the pivotal study which we're hoping [will] be published here soon.
Why did you start with prostate cancer? And what other indications are you looking at?
You start with prostate because there's a clinical dilemma there. It's typically lots and lots of slides, it's typically small core biopsies, and you’re not always seeing [the] small foci of cancer. Using prostate as that first tissue type really made a lot of sense. We’ve since pushed into breast cancer, which is obviously a very high-prevalence cancer. We have other modules for what I call clinical AI applications coming in colon and other tumor types, by prevalence.
We have a suite out today for breast lymph nodes. What the pathologist is doing there is looking for very small metastases that come from the breast tissue into the lymph node itself. It can be very time consuming if they do something that's called an axillary clearance, they’re pulling multiple lymph nodes, dozens and dozens and dozens of slides, that a pathologist has to comb through, looking for very small pieces of cancer. If you don't find any, that patient may get a certain course of treatment, but if there is some cancer there and that cancer is metastatic, it can be very detrimental to the patient downstream.
So that's a tool we think is very valuable. And some of the early studies we've seen, it saves a pathologist, they're saying, 50% of their time, to being more effective and efficient in finding the small metastases.
[With] the things that we're bringing out in our breast suite, detection is okay, but a lot of pathologists can do that. What about grading? What about subtyping? What about mitotic counts? Those are the kind of problems you really want to solve to help pathologists with their workflow.
How do pathologists actually use the tool?
This is human and machine working together. Our studies have shown that pathologists tend to increase their sensitivity by using the AI tool. And so it's not a replacement, it’s that second read. What we've heard from a lot of pathologists, just anecdotally, is that they feel more confident calling something when they have an AI tool available to them.
On something like HER2Complete, what we're seeing with that particular clinical problem, is that with new drugs coming out that actually target very low expression of HER-2 for breast cancer patients, the current modality for pathologists to determine whether that patient is positive or negative for HER-2 is [immunohistochemistry]. And it's designed for very high amplifications, but it's not designed for very low amplifications [of HER-2]. And so what the algorithm really is trained against is both mRNA expression and the IHC expression, to be able to tell that pathologist if there is truly no HER-2 expression at all in that patient, which is important.
Are pathologists embracing the move to digital tools?
[There’s] still a long way to go before the world of pathology is digital, where every pathologist is reading every surgical pathology case digitally, in their primary diagnostic workflow. It's still somewhere in the low-single digits or mid-single digits, percentage wise, as far as diagnoses go, at least in the U.S. [and] a little bit higher in Europe.
Our platform enables a group to go fully digital. We recently announced a partnership with Sonora Quest labs in Arizona. They're taking their many, many pathologists fully digital using the platform, so we really imagine AI tools being part of that.
It's triaging workflow, it allows those pathologists to see the results of the AI even before they open the case.
With things like HER2Complete and different biomarkers, this is ancillary information that they otherwise would never have.
So you're going to have all that information in one place, versus sort of a fragmented, analog workflow today, which is get slide, look at slide under microscope, make some diagnostic decision, send slide back, ask for more stains, ask for more IHC, ask for a recut, this sort of slow, multiple-day turnaround time that ultimately leads to a lot of patient anxiety and oncologist anxiety.
Most hospital labs generally have a scanner. It's just that they're not using those scanners and they would need multiple scanners to scan every single slide they make.
What will it take for hospitals and laboratories to adopt these kinds of solutions?
We see it going in that direction. With [the] new reimbursement codes that are coming out from the AMA, I think we're starting to see that adoption.
Certainly, when there's a bit of a reimbursement involved that helps. We saw that in radiology when CMS really came in and said, okay, if you continue to bill analog codes, we're going to cut your reimbursement by 20%.
In Europe, it's a bit more fragmented. We do work in the U.K. We have a study going right now, a prospective health economic study with the NHS, which was grant-driven, from about a year ago. We work with other sites throughout Europe, it's a bit smaller — smaller hospitals and smaller, more fragmented groups than you get in the United States, but we still have the same sort of adoption happening there as well.
Are there any regulations that you’re watching that could impact the space?
This isn't just about AI or digital pathology, but the VALID Act. Ultimately, the question is, is Congress really going to mandate the FDA oversight of all laboratory developed tests?
We take the perspective certainly as the only company with FDA approval and moving in that regulatory environment, we're open to whatever direction that goes. We think we're very well situated. It's going to be interesting to see what happens. I just don't know if Congress is ever going to get full FDA full oversight of these high-complexity tests, and certainly AI would probably start to fall into those types of things. Today, all of our competitors have research-use-only products and their customers cannot do laboratory developed tests with those algorithms. And certainly with ours, not everything we have is FDA approved. But if Congress does pass something like that in the future, it could be quite monumental.
It’ll be a very interesting space for the next five years, on the regulatory and the CMS side, how they regulate and cover AI algorithms. Certainly, we're not the only ones who will bring things to market but we think will bring a lot of innovative things.
Updated to note the full name of the product is Paige Prostate Detect.